The liver is one of the most complex organs in the body. Its functions include:
- filtering toxins from the blood
- aiding digestion of food
- regulating blood sugar and cholesterol levels
- helping fight infection and disease
The liver is very resilient and capable of regenerating itself. Each time your liver filters alcohol, some of the liver cells die.
The liver can develop new cells, but prolonged over many years can reduce its ability to regenerate. This can result in serious and permanent damage to your liver.
ARLD is common in the UK. The number of people with the condition has been increasing over the last few decades as a result of increasing levels of alcohol misuse.
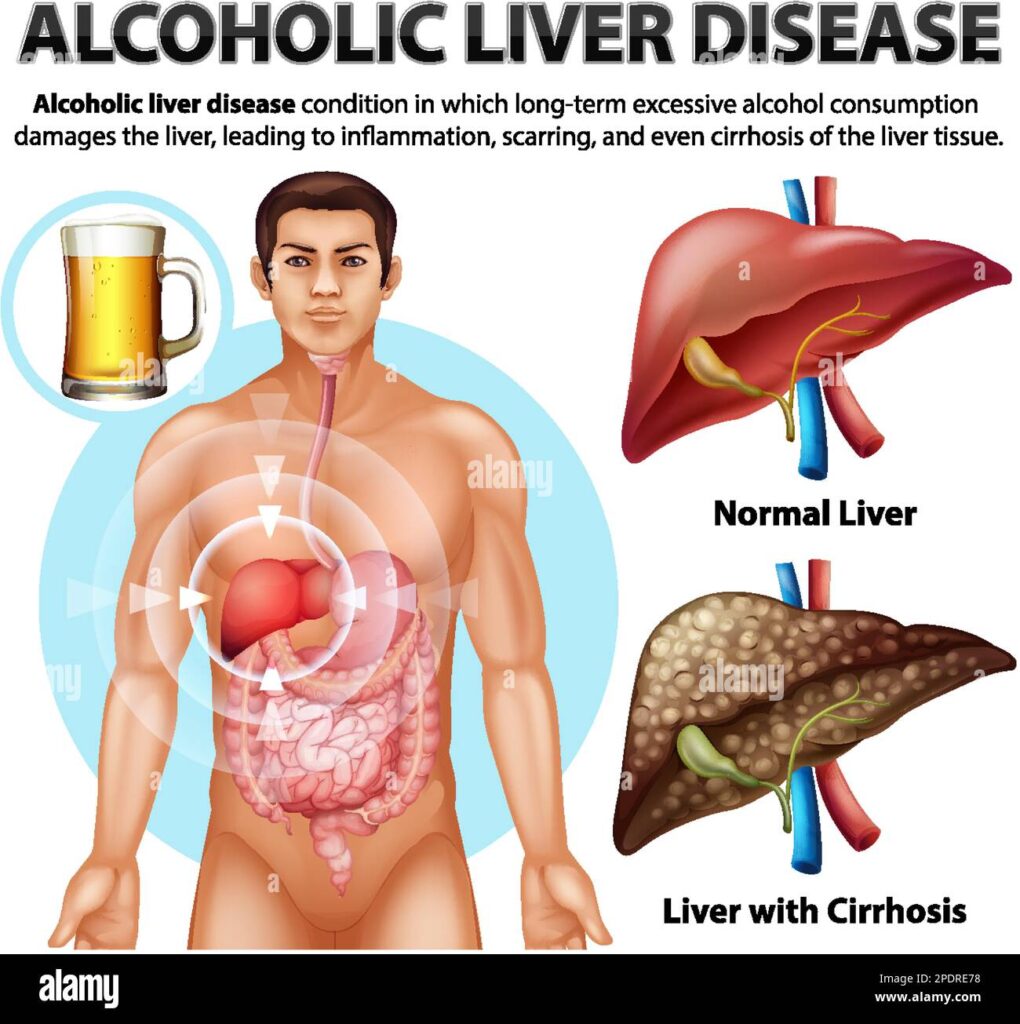
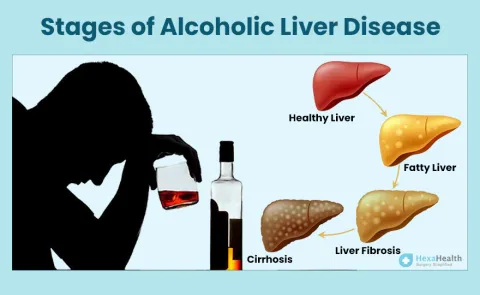
Stages of ARLD
There are 3 main stages of ARLD, although there’s often an overlap between each stage. These stages are explained here.
Alcoholic fatty liver disease
Drinking a large amount of alcohol, even for just a few days, can lead to a build-up of fats in the liver.
This is called alcoholic fatty liver disease and is the first stage of ARLD.
Fatty liver disease rarely causes any symptoms, but it’s an important warning sign that you’re drinking at a harmful level.
Fatty liver disease is reversible.
Alcoholic hepatitis
Alcoholic hepatitis, which is unrelated to infectious hepatitis, is a potentially serious condition that can be caused by alcohol misuse over a longer period.
When this develops, it may be the first time a person is aware they’re damaging their liver through alcohol.
Less commonly, alcoholic hepatitis can occur if you drink a large amount of alcohol in a short period of time (binge drinking).
The liver damage associated with mild alcoholic hepatitis is usually reversible if you stop drinking permanent.
Cirrhosis is a stage of ARLD where the liver has become significantly scarred. Even at this stage, there may not be any obvious symptoms.
It’s generally not reversible, but stopping drinking alcohol immediately can prevent further damage and significantly increase your life expectancy.
Many individuals who consume alcohol heavily progress through these disease types over time:
- Steatotic (fatty) liver. Steatotic liver is the build-up of fat inside the liver cells. It leads to an enlarged liver. Steatotic liver is the most common alcohol-induced liver problem.
- Acute hepatitis. Alcohol-associated hepatitis is an acute inflammation of the liver. There is death of liver cells, often followed by permanent scarring.
- Cirrhosis. Alcohol-associated cirrhosis is the destruction of normal liver tissue. It leaves scar tissue in place of the working liver tissue. In this situation, the liver may stop working correctly.
The liver is a large organ that sits up under the ribs on the right side of the belly (abdomen). The liver:
- Helps filter waste from the body
- Makes bile to help digest food
- Stores sugar that the body uses for energy
- Makes proteins that work in many places in the body. For example, proteins that cause blood to clot.
What causes alcohol-associated liver disease?
Alcohol-associated liver disease is caused by heavy use of alcohol. The liver’s job is to break down alcohol. If you drink more than it can process, it can become badly damaged.
Steatotic (fatty) liver can happen in anyone who consumes a lot of alcohol. Alcohol-associated hepatitis and cirrhosis are linked to long-term unhealthy alcohol use.
Healthcare providers don’t know why some people who drink alcohol get liver disease while others do not. Research suggests possible genetic links, but this is not yet clear.
What is unhealthy or heavy alcohol use?
As of 2023, the National Institutes of Health defines heavy alcohol use as:
- For men, consuming 5 or more drinks on any day or 15 or more drinks per week
- For women, consuming 4 or more drinks on any day or 8 or more drinks per week
In the United States, one standard drink has 14 grams of pure alcohol (ethanol). Some examples include 12 fluid ounces of regular beer, 5 fluid ounces of table wine, and 1 shot of distilled spirits (e.g., gin, whiskey, vodka).
What are the symptoms of alcohol-associated liver disease?
Symptoms of alcohol-associated liver disease may differ depending on how much and how long you have been using alcohol. These are the most common symptoms:
- Often has no symptoms
- Build-up of fat inside liver cells enlarges the liver, causing upper belly (abdomen) discomfort on the right side
- Tiredness and weakness
- Weight los
- Fever
- Weakness
- Abdominal discomfort or pain
- Nausea and vomiting
- Appetite loss
- Poor nutrition
- Weight loss
- Yellowing of the skin and eyes (jaundice)
- Reduced blood flow through the liver due to increased resistance (portal hypertension)
- Enlarged spleen
- Bleeding in the gastrointestinal tract
- Fluid build-up in the belly (ascites)
- Increased infections
- Kidney failure
- Confusion
The symptoms of alcohol-associated liver disease may look like other health problems. Always see a healthcare provider for a diagnosis.
How is alcohol-associated liver disease diagnosed?
Your healthcare provider will do a complete health history and physical exam. Other tests used to diagnose alcohol-associated liver disease may include:
- Blood tests. These include liver enzymes, which show whether the liver is working the way it should and how advanced your liver disease may be.
- Liver biopsy. This involves removing small tissue samples from the liver with a needle or during surgery. These samples are checked under a microscope to find out the type of liver disease.
- Ultrasound. This test uses high frequency sound waves to create a picture of the organs.
- CT scan. This imaging test uses X-rays and a computer to make detailed images of any part of the body, including the bones, muscles, fat, and organs. CT scans are more detailed than general X-rays. Sometimes injecting dye into a vein is done to help show the liver and other organs in the belly (abdomen). Dyes used for CT scans and MRIs are different.
- MRI. MRI uses a magnetic field, radio frequency pulses, and a computer to make detailed pictures of internal body structures. Sometimes injecting dye into a vein is done to help show the liver and other organs in the belly (abdomen). Dyes used for CT scans and MRIs are different.
How is alcohol-associated liver disease treated?
Treatment aims to restore some or all normal function to the liver.
Please stop consuming all alcohol if you have acute hepatitis or cirrhosis. Participation in an alcohol use disorder treatment program can help you achieve this important goal. Sometimes you may also need to change your diet. With complete alcohol avoidance and time to recover, the liver can often heal some of its damage from alcohol, allowing you to return to a normal life. The scarring from cirrhosis is sometimes partially reversible. However, when liver tissue loss is severe enough to cause liver failure, most of the damage may be permanent.
Different treatments are needed for various complications and symptoms of alcohol-associated liver disease. For example, you may need dietary changes, vitamins, salt limit, procedures to shrink swollen veins in the digestive tract, water pills (diuretics), medicines to treat confusion, and anti-inflammatory medicines. In some cases, a liver transplant may be considered
Many people are embarrassed to tell their healthcare provider about their alcohol use. But many forms of help are available. Please discuss your alcohol use truthfully with your provider.
What are possible complications of alcohol a sociated liver disease?
People with alcohol-associated liver disease are at increased risk of also having hepatitis C virus. Others have hepatitis B virus. Your provider will test you for both and treat you if needed.
People with alcohol-associated acute hepatitis or cirrhosis often develop kidney problems, gastrointestinal bleeding, fluid in the belly, confusion, liver cancer, and severe infections.
Key points about alcohol-associated liver disease
- Alcohol-associated liver disease is a common, but preventable, disease.
- Alcohol-associated liver disease is caused by heavy use of alcohol. The liver breaks down alcohol. If you consume more than the liver can process, it can become seriously damaged.
- The effects of alcohol on the liver depend on how much and how long you have been.
- With complete alcohol avoidance and time, the liver can often heal some of its damage from alcohol, allowing the individual to return to a normal life. However, a liver transplant may be needed in some cases.
ALSO VISIT: CVD DISEASE
REFERENCE: VERY WELL HEALTH
